Characterization of EGF-Identified Source
Signatures in Sinus Rhythm and AF
Philipp Sommer, MD; Steven Castellano, PhD; Melissa Kong, MD; David Haines, MD
Background
One mechanism of initiation and propagation of atrial fibrillation (AF) may depend on rapid atrial stimulation from focal sources. Whether arrhythmogenic mechanism at these foci is abnormal automaticity, triggered activity, or microreentry is unclear; however, after activation emerges from these driver sites, fibrillatory conduction results in clinical AF. Electrographic Flow (EGF) mapping visualizes global atrial wavefront propagation in near real-time and has been used to identify areas of centrifugal flow as sources of AF.
Objectives
Characterize EGF patterns of electrical activation across atrial endocardium during sinus rhythm (SR) v. during AF driven by active EGF-identified sources.
Methods
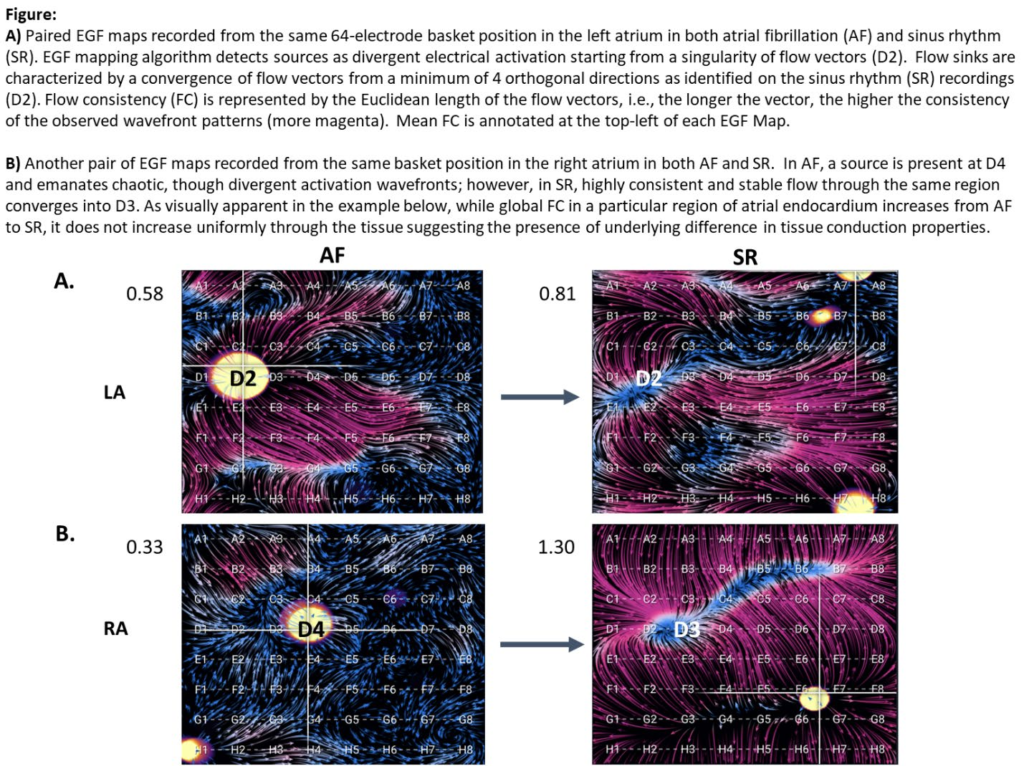
FLOW EVAL-AF is a single-center, prospective study of 10 patients with paroxysmal or persistent AF who underwent EGF mapping with a 64-pole basket catheter. During AF, unipolar electrograms were recorded from the basket for 1 min in 6 biatrial locations per patient and a corresponding set of 1 min recordings were taken from the same locations in SR. EGF algorithm detects sources as origins of excitation from a singularity of flow vectors that emanate from this location. The flow estimation step is a sequence of vector field estimates where Euclidean vector length represents a measure of consistency
of observed wavefront patterns called Flow Consistency (FC).
Results
A total of 10 patients were enrolled. Mean age was 69±10 years; 1 patient was female; mean left atrial (LA) diameter was 4.6±0.5 cm. For the same patient and atrial locations, FC was significantly higher in SR than in AF (0.96±0.11 v. 0.60±0.06, p=0.02). For an individual patient, areas of high FC in AF were not correlated to areas of high FC in SR. Eleven areas of AF source activity (SAC) were detected—7 in LA and 4 in RA. Mean SAC was 32±0.09%. In 8 of 11 (73%) locations where active sources were identified during
AF, electrographic flow converged into a “sink” region at a location within 1 electrode distance of the source; 5/7 (71%) were in LA and 3/4 (75%) were in RA. Mean SAC was higher among sources that became sinks compared with those that did not (34±10% v. 27±4%, p=0.14).
Conclusions
Electrographic flow patterns vary significantly in both magnitude and direction depending on the rhythm. AF sources emanate flow during ongoing AF, but when inactivated during SR, appear more as flow sinks possibly due to surrounding abnormal substrate with slow and/or anisotropic conduction due to arrhythmogenic remodeling.
